Contact Admission
International Collaboration
Dr. Pham Hung Van shared more scientific information about coronavirus causing pneumonia outbreak Covid -19
Today I would like to send more to my friends about the scientific information about the coronavirus that causes the new pneumonic plague named CoVID-19.
Has coronavirus previously caused illness in humans?
Coronavirus is a virus that mainly infects wildlife, including domestic animals like pigs. However, since 1962, the coronavirus strains that cause common cold have been discovered in humans and this coronavirus is still occasionally detected from patients. In 2003, there was a line of coronavirus causing severe acute pneumonia in humans, which we call as SARS (Severe Acute Respiratory Sydrome), which in the elderly over 65 years old, the mortality rate is up to 50%. The causative agent of SARS has been identified as a strain of coronavirus originating from civet and epidemic originating from Guangdong, China. Fortunately, thanks to the efforts of the health sector in the world, this disease was stopped and disappeared in July 2003 after causing disease in 8422 with 916 deaths (11% mortality). Then in September 2012, another serious respiratory infection was discovered, and the agent was identified as coronavirus but was of camel origin. As of December 2019, the world had 2468 cases of Middle East pneumonia with 851 deaths (relatively high rate of 34.5%). This unknown disease has disappeared yet so medicine is still vigilant for a comeback.
From December 2019 in Wuhan city in China (China) an outbreak of acute pneumonia again broke out, which not long after scientists identified the cause as also a new strain of coronavirus that today is named. is CoVID-19 (CoVI is a coronavirus, D is a disease, and 19 is 2019) derived from a bat. By February 16, 2020, according to data published by the World Health Organization (WHO), the disease had spread throughout China with a total number of confirmed cases of 51,174 (death was 1666). Not only that, the disease also spread to 25 countries with 683 people infected (3 died). Particularly in Vietnam, up to now, 16 people have been identified and no deaths have been reported. In terms of mortality it is generally around 2%, but mainly in the old age group with underlying diseases such as diabetes, cardiovascular disease, respiratory illness and death not directly caused by virus but by underlying disease. becomes more severe.
Current course of CoVID-19 pneumonia
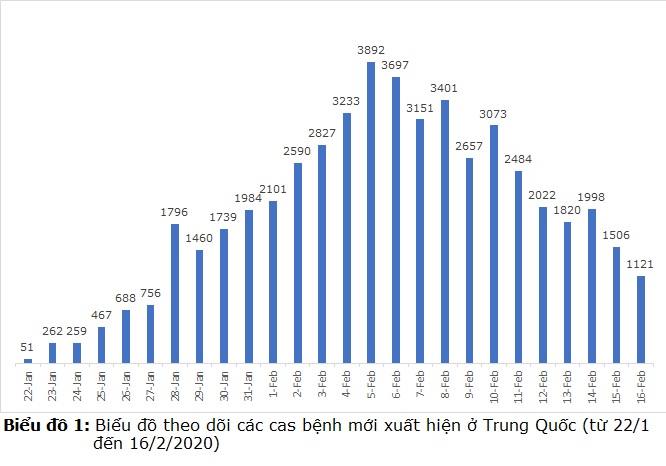
The press often only reports on the number of people infected and fatal by CoVID-19; So many people, especially non-professionals, find it quite confused. For example, if you read the information in the newspaper, "CoVID-19 so far has caused 51,857 diseases and 1669 deaths", many people will feel insecure because of the number of people infected and dying from CoVID- 19 more and more. However, if you look at the chart of the progression of the disease caused by CoVID-19 (chart 1, drawn from official numbers from WHO, but only for reference), you will see that the disease is gradually receding with the number of new cases is decreasing. Thus, the epidemic countermeasures of the world health are working and we can fully believe that CoVID-19 pneumonia is receding.
Mechanism of infection of 2019-nCoV and how to prevent it
Why CoVID-19 spreads from bats to humans is still a mystery that scientists have yet to explain. It is also possible that someone who ate a bat infected with CoVID-19 and then infected with the virus, could also be transmitted through an intermediate host. Once infected, the virus will spread from person to person through droplets shot from an infected person who coughs or sneeze and then directly into others through the nose or mouth. The reason why CoVID-19 is only present in large or medium droplets when an infected person coughs or sneezes, is because, like the coronavirus that causes SARS or other coronaviruses, CoVID-19 is quite large in size up to 165nm. can only be on large and medium-sized droplets, not in droplets to fly as far in the air as influenza virus (size 65nm). That is why we can prevent this infection with a mask covering the nose and mouth is enough. Any mask is fine, medical is fine, N95 or 3M is fine, multi-layer fabric masks are fine, even homemade multi-layered masks are fine. The main thing is to stop the drops of the other person or go ahead coughing, sneezing, spitting clinging to. Why any mask works, that's because we only need a mask to help prevent drops from being shot into the nose or mouth by the sick person, not to prevent the virus because there is no mask, including medical masks. get virus. Then will the droplets sticking to the outside of the mask make the virus crawl inside if the mask is absorbent? Even more impossible because the virus does not know cows, even bacteria, even if they are mobile, cannot crawl in, the droplets will dry and will follow the mask into the trash and be treated. Conversely, if using expensive masks or the price is pushed up due to scarcity, users often tend to use them again and thus increasing the risk of infection due to the virus sticking to the outside, there is a chance of infecting the nose and mouth. use. In addition, wearing a mask also has a very humanistic significance for people, that is to prevent us from getting sick and coughing, sneezing, and sneezing will avoid splashing drops on others. Currently we wear masks in the habit of being dustproof, not anti-epidemic. If a mask is worn, the mask cannot be reused, and while wearing and removing the mask, we must not allow our hands to touch the front of the mask. If done so, we must use at least 3 masks every day, and with the current scarcity of masks, how can we have enough masks to use. Therefore, we think that if there is a real epidemic going on, we should refrain from going out or going to public places. If you have to go out, you must use a mask properly.
In addition to a mask, a very important way to prevent the spread of infection is to wash your hands frequently as hands are the most important source of infection. Hands infected by coughing or chewing gas will infect the infected materials such as doorknobs, stair hands, elevator buttons, intimate handshakes, daily household cups, etc. Hospital or restaurant / hotel ... and from there it spreads to others because they will touch these places ... then accidentally bring it to their mouth through the mouth, through eating ... That's why the method of washing hands is often After going out to public places, hospitals, hotels, cafes ... is very necessary to avoid infection, we must pay attention and implement it thoroughly when an epidemic occurs. Coronavirus is very easy to kill by 70% alcohol, alcohol mixed with isopropanol, or adding chlorhexidine all kill coronavirus. It is not necessary to find and buy hand sanitizer that is advertised on the Internet, but pay for it if you do not qualify.
Mechanism of pneumonia of CoVID-19 and clinical evidence for identification
The agent 2019-nCoV penetrates the respiratory mucosa cells through their spiny structures that attach to the receptors on the surface of the mucosal cell and then penetrate the cell, releasing their RNA for synthesis. the components of the virus then the complete virus. Therefore, the virus has damaged the respiratory mucosal cells causing diseases, mainly pneumonia. There has been no documented mechanism of pathogenesis of the type SARS, ie, pulmonary parenchymal destruction by storming cytokines from the body's excessive immune response. However, there are also severe cases that can lead to death, especially in elderly patients with underlying respiratory, cardiovascular, or metabolic disease. Most cases heal after 7 to 14 days of hospital treatment. Recovery means that the patient has antibodies and no longer presence of virus in the respiratory tract through real-time PCR test results performed for 2 consecutive days.
The most common clinical signs of pneumonia caused by CoVID-19 are cough (usually a lot of cough), fever, soreness, possible diarrhea, more severe cases may be difficulty breathing and chest pain. . However, these signs can also appear in pneumonia caused by other viral agents or even bacterial agents. Therefore, if only based on clinical symptoms to identify a person with pneumonia caused by CoVID-19 is not possible. Pneumonia can only be identified as caused by CoVID-19 once the test results of throat swab, or posterior nose swab, or blood sputum or blood in the acute phase has found CoVID-19 by the real-time PCR assay. standard.
Principles of treating CoVID-19 pneumonia
In fact, there is currently no specific antiviral treatment for CoVID-19. There is also ongoing clinical trial using Remdesivir, an analogue of the nucleotides with a mechanism that prevents viruses from synthesizing their RNA. Chloroquine has also been noted for its mechanism of preventing viruses from translating RNA for the synthesis of their proteins. However, all are in the research phase and have not been approved by the FDA.
Thus, the treatment of pneumonia caused by CoVID-19 is based on the principle: (1) Supportive treatment for the patient such as oxygen if breathing is difficult, electrolyte replacement if there is a disorder, and nutritional supplements if necessary ... (2) Monitoring to detect bacterial superinfection for timely antibiotic treatment. In most cases, just the above two solutions will be sufficient.
Diagnosis of pneumonia caused by CoVID-19
To identify CoVID-19 agent, standard real-time PCR test must be performed and this test has been provided with detailed instructions on website by CDC and WHO. A very favorable point for using real-time PCR in detection of CoVID-19 is that the CoVID-19 genome is very stable and does not differ between different patients as well as the locality. Therefore, laboratories can perform this test based on the priming sequences and probes provided by CDC or WHO, without having to redesign to suit the pathogen. In principle, laboratories have real-time PCR facilities, obtain the necessary materials according to CDC or WHO guidelines, have biosafety level 2, and have a list of detectable tests. A viral, bacterial or fungal agent may perform this test. However, because currently, pneumonia caused by CoVID-19 is classified as an emerging epidemic risk agent, there are only 3 places: Central Institute of Hygiene and Epidemiology, Pasteur Institute of City. HCM City, and Nha Trang Pasteur Institute are entitled to publish the results [+]. Therefore, other laboratories, even if they have the capacity, have to wait for the approval of the state to conduct testing.
Currently, the need for a CoVID-19 test is high. However, in order to help prevent CoVID-19 testing from being overloaded, doctors should only recommend CoVID-19 testing in patients with symptoms of pneumonia and weakness. epidemiological factors such as having traveled to or visited epidemic areas, or had contact with sick patients, or sat on an airplane in about 2 seats around the patient. In addition, testing is also possible in pneumonia patients but cannot rule out epidemiological factors. However, according to the current regulations, the clinic can not order tests, but must refer the suspected patient to a specialized clinic for CoVID-19 designated by the government, not take the specimens directly. to submit for testing.
What is the progression trend of CoVID-19 pneumonia?
Scientists think there may be 3 trends: (1) The disease will recover but will turn into endemic like seasonal flu due to current H1N1; (2) The disease will become a pandemic worldwide such as the 1918 Spanish flu with high morbidity and mortality; (3) Or after the peak of the epidemic, the disease will gradually subside and disappear like SARS in 2003.
From the point of view of a clinical microbiologist, after analyzing the virological properties as well as analyzing the transmission mechanism as well as the pathogenesis mechanism of CoVID-19, I think the disease will progress according to the same trend. such as SARS, which means that after the peak of the epidemic, the disease will gradually recede and disappear completely, by July 2020, possibly a few months earlier. There are reasons for this:
1. Like the SARS coronavirus, CoVID-19 has a regular wildlife host and only causes illness to humans by accident. Therefore, if we can stop the epidemic from spreading to humans, the disease will disappear, but it cannot be endemic. This has been proven through the SARS epidemic. After the epidemic peak in March and April, the translation gradually retreated until July 2003.
2. There will be no endothelium because it is cured that the patient has immune protection but no longer carries the virus in the respiratory tract. In addition, with the method of isolating the source (isolating the patient until the disease is cured and testing for 2 consecutive days negative, isolating the person at risk within 14 days), surely there is no epidemic spreading into the community and thus will reduce the risk of the virus finding a permanent carrier as well as long-term spreading in the community.
3. When spring is over, the temperature in China will get warmer, so that CoVID-19 will no longer be present in the outside environment, so human-to-human transmission will cease. And on the same reasoning, I think CoVID-19 will not spread strongly in tropical countries, but will gradually reduce the spread.
On the question of whether SARS will come back, and if CoVID-19 disappears, will the pneumonia caused by CoVID-19 return? In my opinion it is quite possible, but not because the agent hidden in the host is human, but again by accident by humans because of their preferences to eat wild animals. The return will be more difficult, however, as populations, especially at-risk populations, have previously had specific immunity.
Source: facebook Dr. Pham Hung Van
Other news
- May 19 morning: Vietnam has 31 new COVID-19 cases, the Ministry of Health consults with a 'record' of 20 severe cases ( 08:51 - 19/05/2021 )
- May 06, an additional 8 cases COVID-19 at the Tropical Disease Hospital Central ( 10:10 - 06/05/2021 )
- This morning 5-5, Vietnam has no new cases of COVID-19, more than 602,000 more globally ( 14:29 - 05/05/2021 )
- On the morning of May 3, Vietnam did not record a new case of Covid-19 infection ( 07:56 - 03/05/2021 )
- UPDATE KNOWLEDGE ON HOW VACCINE COVID-19 WORKS ( 10:28 - 20/03/2021 )
- On the morning of March 1, no cases of COVID-19, 210 patients undergoing treatment were negative ( 08:28 - 01/03/2021 )
- On the morning of February 25, there was no new case, a patient with very severe COVID-19 ( 08:35 - 25/02/2021 )
- How to wear a Mask properly ( 09:01 - 22/02/2021 )
- 39 provinces and cities let students stop going to school ( 09:47 - 17/02/2021 )
- COVID-19 'brutally exposes' the technological gap ( 15:29 - 30/01/2021 )