Contact Admission
International Collaboration
Abrocitinib: A New Direction in the Treatment of SAPHO Syndrome
While many treatment approaches for SAPHO syndrome remain a race between hope and challenge, a recent report in JAMA Dermatology has opened a new door: abrocitinib – a selective JAK1 inhibitor – demonstrated marked clinical efficacy in a representative case.
SAPHO Syndrome – A Complex Clinical Puzzle Yet to Be Solved
SAPHO, an acronym for Synovitis, Acne, Pustulosis, Hyperostosis, and Osteitis, is a rare and challenging systemic inflammatory disorder. The disease lacks standardized international diagnostic criteria and a unified treatment protocol. Most current therapies—such as NSAIDs, bisphosphonates, and DMARDs—provide only partial relief.
Even targeted therapies like secukinumab (an IL-17 inhibitor), once considered promising for pustular dermatoses, have shown limited success in certain SAPHO cases. Patients may continue to experience persistent pruritus and pustules despite guideline-based treatment.
From Frustration to Hope: Abrocitinib and a Selective Targeted Approach
In this context, a new therapeutic direction has emerged: abrocitinib, a selective Janus kinase 1 (JAK1) inhibitor. JAK1 is a key intracellular kinase involved in transducing inflammatory cytokine signals. Unlike broad-spectrum JAK inhibitors such as tofacitinib, abrocitinib acts selectively on JAK1, allowing for more precise modulation of inflammation with a potentially better safety profile.
Clinical Case: A Real Story, Real Results
A woman in her early 50s was initially diagnosed with pustular psoriasis of the palms and soles. After two months of unsuccessful treatment with secukinumab, she was re-evaluated and diagnosed with SAPHO syndrome based on:
-
Recurrent anterior chest pain
-
CT scan showing lesions in the clavicle and sternum
-
Elevated ESR
-
Positive HLA-B27
After ruling out contraindications, she was prescribed abrocitinib 100 mg orally once daily. The results were remarkable:
-
Complete pustule clearance after 16 weeks
-
Rapid itch relief within 1 week
-
Chest pain resolved after 8 weeks
-
ESR normalized
-
No progression of joint damage observed on follow-up CT
-
No adverse effects reported
Abrocitinib, as a selective JAK1 inhibitor, presents fewer side effects compared to pan-JAK inhibitors. Its efficacy across both cutaneous and osteoarticular symptoms—the two hallmark challenges of SAPHO—suggests its potential not only for symptom control but also for altering disease progression if introduced timely and appropriately.
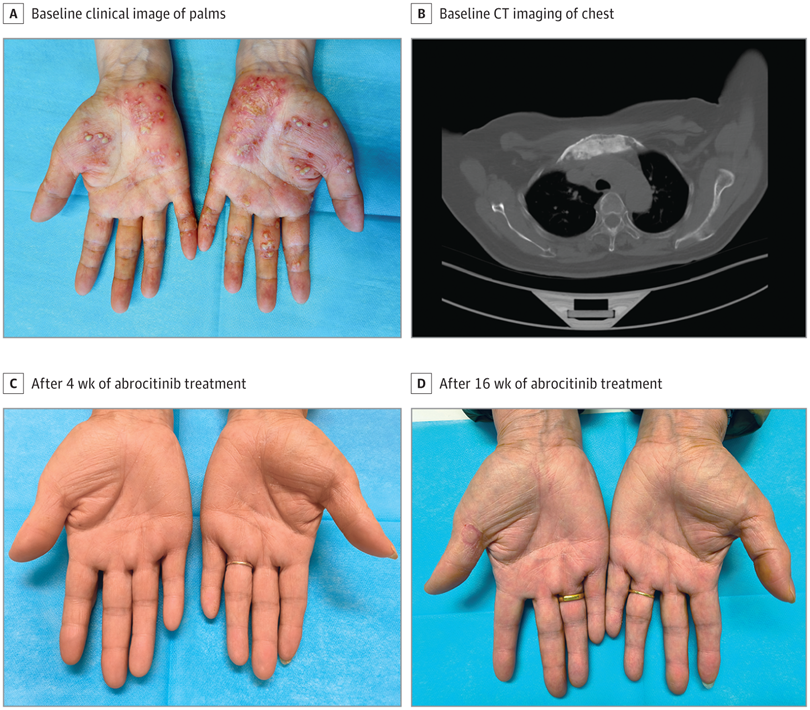
Clinical course and CT imaging of the patient before and after treatment with abrocitinib
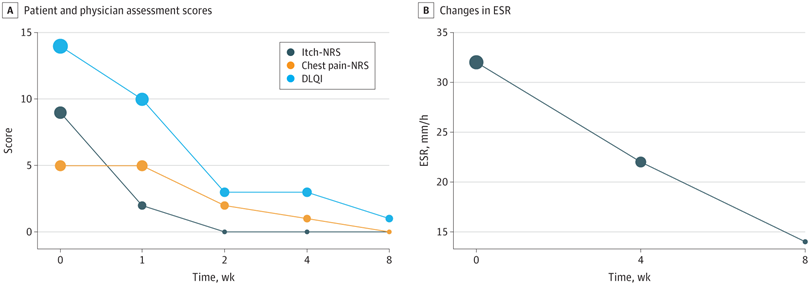
Assessment of itch, chest pain, quality of life, and erythrocyte sedimentation rate (ESR) during follow-up
Author’s Note: This Is Only the Beginning
While the results are promising, it is important to recognize that this is still a single case report. Larger, controlled studies are needed to confirm the efficacy, safety, and clinical applicability of abrocitinib in the treatment of SAPHO syndrome.
This article is based on the study titled “Treatment of Synovitis, Acne, Pustulosis, Hyperostosis, and Osteitis Syndrome With Abrocitinib”, published in JAMA Dermatology on May 7, 2025, by Dawei Huang and colleagues.
SAPHO syndrome is difficult to diagnose—and even harder to treat. However, every small step forward in therapy, such as in this case, contributes to renewed hope for patients and the medical community. By continuously updating ourselves on emerging therapeutic options, we can move faster toward personalized and effective treatments.
???? Read the full article in JAMA Dermatology here
Other Case Report
- Viêm da tiết bã, dấu hiệu rối loạn hàng rào biểu mô hệ thống ( 07:44 - 08/11/2025 )
- Artificial Intelligence in Surgery ( 14:48 - 06/09/2025 )
- Identifying Collagen Vascular Disease Through Persistent Skin Lesions ( 10:29 - 19/06/2025 )
- MỘT TRƯỜNG HỢP ABSCESS VÙNG HANG VỊ- CĂN BỆNH HIẾM GẶP- ĐƯỢC ĐIỀU TRỊ THÀNH CÔNG TẠI BỆNH VIỆN TÂM TRÍ CAO LÃNH ( 09:34 - 09/05/2025 )
- Phẫu thuật Mitrofanoff: 40 năm nhìn lại. ( 08:35 - 11/04/2025 )
- SỬ DỤNG MẬT ONG HOA TRÀM CHIẾU XẠ TRONG ĐIỀU TRỊ LOÉT TÌ ĐÈ ( 08:21 - 28/03/2025 )
- Chronic Progressive Pink-Yellow Papules and Nodules in a Middle-Aged Man ( 09:02 - 24/09/2024 )