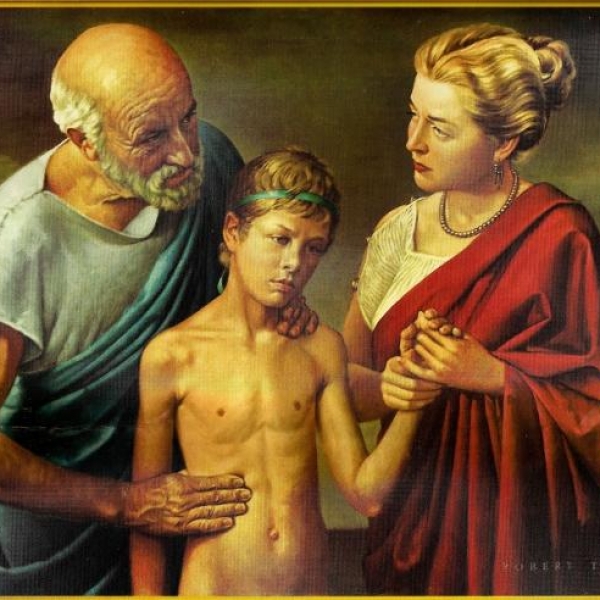
Medical staff in Newark, New Jersey took the patient into an ambulance last month. Photo: NYTimes.
In March, the US Centers for Disease Control and Prevention (CDC) advised emergency response technicians to be cautious when taking actions that could spread nCoV, including CPR.
In essence, chest compressions are the act of close contact. Every time a medical staff presses the chest, the forced air escapes from the patient's lungs, potentially carrying Covid-19 pathogen.
After the CDC issued the recommendation, many states did not change their CPR policy. However, in New Jersey, the second highest number of nCoV infections in the US, many health facilities apply the new rules. At the University Hospital in Newark, New Jersey, which coordinates ambulances for 911 calls, many medical staff were infected with nCoV, 7 died.
Terry Hoben, the hospital's emergency services coordinator, noticed the numbers: Before the Covid-19 outbreak, the hospital's ambulance fleet received about three calls a day about cardiac arrest. In April, they recorded an average of 14 cases a day. Hoben suspects this spike is associated with Covid-19 and that cardiac arrest is the terminal stage of the disease.
If that is true, the health care workers are at high risk, as chest compressions spread the high concentration of virus out. Hoben regulates that health workers do not do CPR from 11/4, except for cases such as patients under 18 years old, pregnant women and people drowning.
In other cases, if the ECG shows a straight line, indicating that the heart has stopped beating, the medical staff determines that the victim is dead, no CPR is required. At least 10 of the 14 cardiac arrests they recorded daily fell into this category.
Medical worker John McAleer, 51 years old, was called to the ambulance of a 90-year-old woman with nCoV infection. A few weeks ago, when New Jersey was not heavily affected by the epidemic, in cases like these, McAleer and his colleagues were able to use a chest defibrillator and could use a defibrillator, although studies show that only about 1 -3% of people who fall into this situation can be saved.
The chest compressions will almost certainly not help the old woman survive. Even though the medical staff wore goggles, splash masks and masks, they could not 100% guarantee they would not get the virus.
But trained medical personnel need to do their best to save every life. Now, they must put their health on top of the patient. "It's annoying because this goes against everything we've been taught," McAleer said.
Angel Garcia, a colleague who accompanies McAleer, speaks with the patient's family. They asked many questions and Garcia had to do her best to explain why they hadn't put in more effort to save her grandmother.
"This is something we have never done before. It is scary. This issue also entails a moral debate," Hoben said. "We are not taking this lightly."
On a recent Sunday morning, medical officer Mark Radice was called to an ambulance for a man. When the electrocardiogram displayed a straight line, Radice did nothing more than determine he was dead. The patient's family was very angry, the medical staff left when the police arrived.
"Normally we would try to do CPR, but I understand why that policy exists," Radice said. Many people without medical knowledge believe that CPR is the manipulation of up to 70% of patients, as is often portrayed on TV series. "I can confirm the truth in real life is not like it was on the film," said Richard Kamin, medical director of Connecticut Emergency Services.
After much debate about the CPR regulation, Hoben's department is discussing whether to allow health care workers to continue doing CPR but limit the time to perform the operations.
But last month, when Hoben stressed that hospitals need to take more drastic measures to protect medical staff, he said: "Save one life, but there is a risk of losing 5. It doesn't fit. physical".
Phuong Vu (According to NYTimes)
Source
: vnexpress.net
https://vnexpress.net/nhung-bac-si-khong-the-het-long-cuu-benh-nhan-4098001.html